
Trying to eliminate cohorts of waiting list patients is too simplistic says Rob Findlay.
Analysis produced for Health Service Journal by Dr Rob Findlay, Director of Strategic Solutions at Insource Ltd and founder of Gooroo Ltd
The Elective Recovery Plan set out a number of ambitions, including: “That the waits of longer than a year for elective care are eliminated by March 2025. Within this, by July 2022, no one will wait longer than two years, we will aim to eliminate waits of over 18 months by April 2023, and of over 65 weeks by March 2024.”
That July ambition has been “virtually” achieved (i.e. narrowly missed) with 2,777 patients still waiting longer than 104 weeks at month end. All of the remaining ambitions will be missed too. Here’s why.
Zero tolerance targets
Back in 2013, the Department of Health introduced a non-statutory zero tolerance of any RTT waits of more than 52 weeks, with heavy financial penalties for any breach. The rationale? It is unsafe and unfair to keep tiny numbers of patients waiting excessive lengths of time when nearly all other patients are being treated much more quickly.
Zero tolerance targets work well when they are a distant backstop, well beyond reasonable patient choice to wait longer, which was the case in 2013. The statutory standard was (and still is) for 92 per cent of the referral-to-treatment (RTT) waiting list to be within 18 weeks; in 2013 this standard was consistently met at national level and even went as low as 15.8 weeks – a waiting time that seems miraculously short today.
Even when waiting times were that short, the zero-tolerance target was never completely achieved. At its best, in November 2013, there were still 214 patients reported as waiting longer than 52 weeks across England. This alone tells us that none of the ambitions in the Elective Recovery Plan will be fully met, but you could (as I did) argue that it was still a worthwhile target that served a valuable purpose at the time.
But what happens when a zero-tolerance target is not a distant backstop, but used as a policy tool to drive headline reductions in waiting times? This is when it runs into trouble.
Over the years, various statutory RTT standards have been created to drive down English waiting times. None of them were zero tolerance targets that applied to 100 per cent of patients; instead, the Department of Health (who were in charge of this at the time) required 90-something per cent compliance. The reason is clearly and correctly explained in the official statistical press notices. “These proportions leave an operational tolerance to allow for patients for who starting treatment within 18 weeks would be inconvenient or clinically inappropriate.” Or to put it another way, nobody wants patients to be coerced into treatment because their hospital has a target to meet.
If you try to drive down waiting times using zero tolerance targets, you have to create extra rules to define all the reasonable exceptions and protect patients. But every exception creates a potential loophole, and there is the further risk that exceptions might be invented or used to serve the provider rather than the patient. This has been the experience in Scotland, where the many exceptions have in the past been exploited with considerable enthusiasm by hospitals trying to limbo under the targets.
We are seeing similar things now in England, where the elective recovery ambitions already come with the footnote “Some patients will choose to wait longer”, and provider-oriented exemptions are being created for ‘complex’ services that cannot easily move patients to other hospitals.
But let us be clear: patients do not choose to wait years for treatment rather than, say, 18 weeks. If after 50 or 100 weeks of waiting they are asked if they would like to drop everything and come in next week or travel to a hospital some distance away, they may decline, but that is not the same thing.
So, before we go any further with zero tolerance targets and their contestable exceptions, would it not be more straightforward and transparent to have a tried-and-trusted 90-something per cent target instead?
Cohort management and ‘tip-ins’
Most of the NHS, encouraged by the centre, takes a very direct approach to RTT waiting time targets. Want to eliminate 78-week plus waiters by the end of April 2023? Then draw up a list of all the patients who are potential breaches by that date, and get those patients in. This approach is considered more sophisticated than simply tracking actual 78-week waiters over time, because now we are anticipating those patients who will ‘tip in’ to the 78-week-plus cohort between now and the deadline.
Here is a thought experiment to demonstrate why this approach does not work.
Imagine it is the end of May 2022. The end of April 2023 is 48 weeks away. Therefore, any patient who has waited longer than 30 weeks now, is a potential 78-week breach at the end of April. These are the patients we will need to see and treat between now and then, and this is the source of NHS England’s warning that “There are over a million patients who, if the NHS doesn’t treat, will tip into [the 78-week breach], so it’s a huge cohort of patients.”
We track this cohort of potential 78-week breaches closely and get off to a cracking start in the early months. At the end of August, the size of the potential breach cohort – which by now is the 43-week-plus waiters – has better than halved. At this rate we’ll clear them all by Christmas!
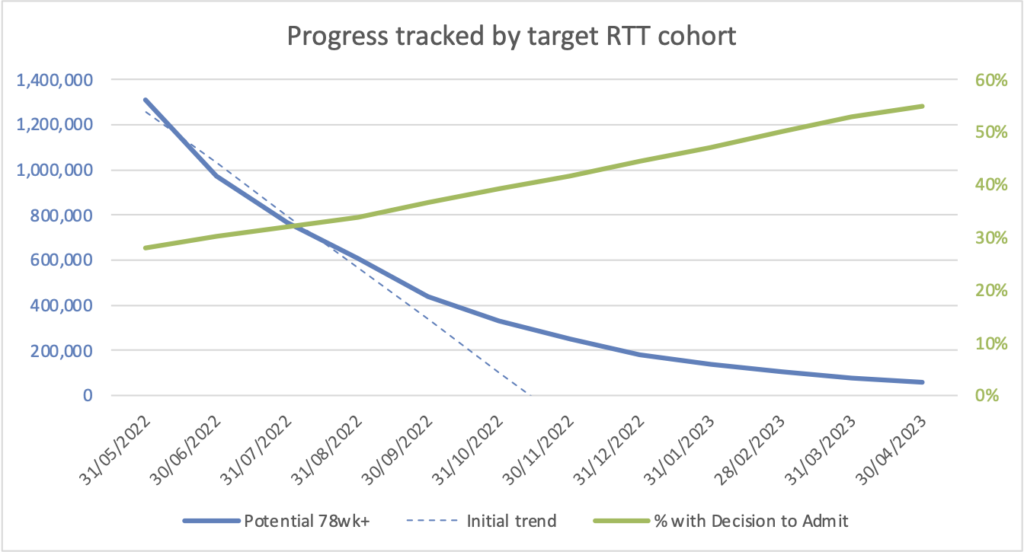
But as autumn sets in, the rate of improvement starts to flatten. Is it because we have cleared mostly outpatients so far, leaving the heavier case-mix of admitted patients still to tackle? The monitoring data suggests this: the proportion of the list with a decision to admit has been going up. We must redouble our efforts before winter comes!
Alas, improvement continues to flatten over the autumn, and as winter arrives it becomes clear that we won’t achieve the target. At the end of April, we review our result. Although we didn’t get to zero, we did clear 95 per cent of the cohort which is not at all bad. Let’s chalk it up as “virtually achieved”.
Now here is the twist. Throughout this thought experiment, nothing actually changed. There was no improvement in either the size or the shape of the waiting list, which are the two drivers of waiting times. The number of 78-week plus waiters did not improve either. Every point on the chart was based on the same waiting list snapshot, which is for the end of May 2022 and shown in the chart below:
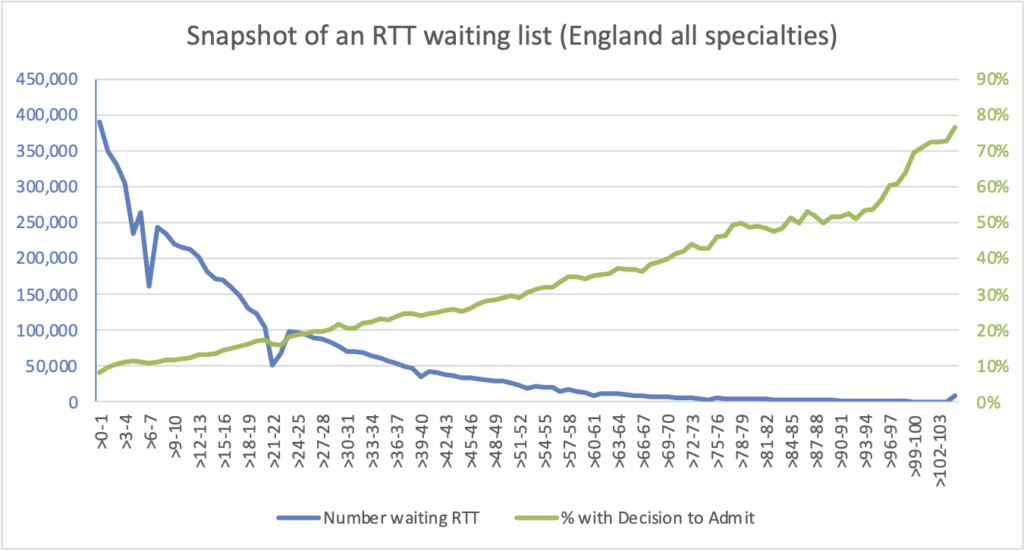
As time went by, the potential 78-week breach cohort was a smaller and smaller slice of the tail on this waiting list: over 30-week waiters at the end of May 2022, over 43 week waiters at the end of August, over 61 weeks at New Year, and of course over 78 weeks at the end of April 2023 deadline. All of the apparent improvements were caused by the dwindling number of patients in this ever-diminishing tail.
Would it be better simply to track the number of 78-week waiters over time, and ignore the potential ‘tip ins’? It would, because this does contain a bit of information about the shape of the waiting list, and it is understandably a popular approach. But again, there are pitfalls, because if the underlying pressures on waiting times are not being addressed, then at some point local services will start to find it impossible to make continued progress on 78 week waits without compromising clinical priorities.
The moral of this story is that tackling waiting times means tackling the causes of waiting times: reducing the size of the waiting list by keeping up with demand, improving the shape of each list with safe and fair patient scheduling, and ensuring that pressures are not allowed to persist in some services while being reduced in others. Or to put it another way, successful and sustainable waiting time reduction will only be achieved by managing the whole waiting list continuously. By contrast, the cohort tracking approach leads us astray.
Our thought experiment raises other concerns too. Most of the waiting list was left relatively unmanaged while we focused on the potential breach cohort. The focus shifted more and more towards routine patients with a diagnosis and decision to admit, despite the greater clinical risk among the undiagnosed. Instead of careful capacity planning to ensure the target was safely achievable without compromising clinical priorities, it was simply assumed that it was.
More fundamentally, I worry that the emergence of 100 per cent targets as the policy instrument for driving down waiting times, and the widespread adoption of direct but simplistic methods for achieving them operationally, signify an atrophying of understanding and skills around waiting list management that began with the introduction of RTT waiting times in 2007 and has since spread to all levels of the NHS.
If elective recovery is to be achieved safely and sustainably, then we need to regain and build upon these skills, and soon.
